
Kidney Collaboration
An estimated 37 million people in the United States have some form of chronic kidney disease, and every year 100,000 of them die while undergoing kidney dialysis. It’s a major public health problem that costs the U.S. government billions in Medicare payments, but University of Arkansas researchers Jamie and Christa Hestekin – in conjunction with a kidney doctor in Southern California – are working to revolutionize the treatment options available.
Of the approximately 15% of U.S. adults who will face this diagnosis, about 100,000 people will develop end-stage renal disease. Treatment options for this group – hemodialysis, peritoneal dialysis or kidney transplant – have not changed significantly over the past 50 years. According to the Centers for Disease Control, the average duration of patient survival on dialysis is approximately seven years, but most patients have to wait 10 years to receive a donated kidney. As a result, many people die waiting for a kidney transplant.
The U.S. government spends more than $100 billion in Medicare payments – almost 10% of Medicare’s annual budget of $1 trillion – to care for patients with kidney disease.
If the Hestekins’ collaboration is successful, their techniques will offer hope for something better than the traditional treatment methods, such as dialysis or transplantation, and greatly improve peoples’ qualities of life.
“We’re trying to improve the lives of patients with end-stage renal disease by giving them more freedom and a better treatment method, so they can live healthier, happier lives,” says Christa Hestekin.
The Power of Electrodeionization
Though most people haven’t heard the term “electrodeionization,” it’s a regular part of Jamie Hestekin’s vocabulary and day-to-day work as a chemical engineering professor.
Several years ago, a decade into his career at the U of A, Hestekin received a call from Ira Kurtz, a prominent nephrologist in Southern California. At the time, Hestekin had no way of knowing that Kurtz’s call would change the direction of his work and eventually dominate his research agenda.
Electrodeionization removes or separates ions (electrically charged molecules) from water by applying an electrical charge to a specially designed membrane. This process is primarily used in water treatment.
Before Kurtz’s call, Hestekin had used the technology to remove ions from grape juices, cells from biofuels, and organic acids from fermentations. More recently, he was a research consultant for fracking companies, applying the process to the removal of environmentally hazardous particles from wastewater.
As Distinguished Professor of Medicine and Chief of Nephrology at UCLA Health, Kurtz is a leading basic researcher on the structural biology and physiology of the human kidney. He focuses on proteins that transport various ions in renal and extrarenal tissues. In the kidney, ion transporters play an important role in helping determine the final chemistry of urine.
As Kurtz emphasizes, the human kidney is not a simple filter. It functions like a computer, sensing the chemistry of our blood and keeping it constant, despite all the chemicals that food and beverages introduce into the blood. How the kidney accomplishes this is a major focus of his research.
In addition to studying the ion transport process in the kidney, Kurtz, along with the US Kidney Research Corporation, had been investigating a new, radical idea.
“I’d been thinking about creating an artificial kidney,” he said. “So, I looked around to see what was out there. There were a few efforts, but I could see they weren’t going to work ultimately.”
Kurtz started exploring techniques that could transport critical ions, such as sodium and potassium, without using dialysis. The device he envisioned would be implantable and therefore couldn’t use water, a dialysate or a dialyzer, which are currently used to treat patients. He ultimately landed on electrodeionization as a technology that could potentially work. After looking at several researchers around the country with a background in this process, he called Hestekin.
A Chemical Computer
Kurtz likes to say that the kidney is more complex than a 747. Its microanatomy is particularly intricate, containing roughly a million nephrons, each of which is responsible for filtering and transporting ions and other substances that will end up in the urine. Each nephron contains a filter, called a glomerulus, and a tubular transporting part that is further subdivided anatomically and functionally into about 15 segments that contain different cell types. Kidneys also have nerves, arterial and venous blood vessels, and lymphatics that, along with the nephrons, are configured in a complex three-dimensional structure.
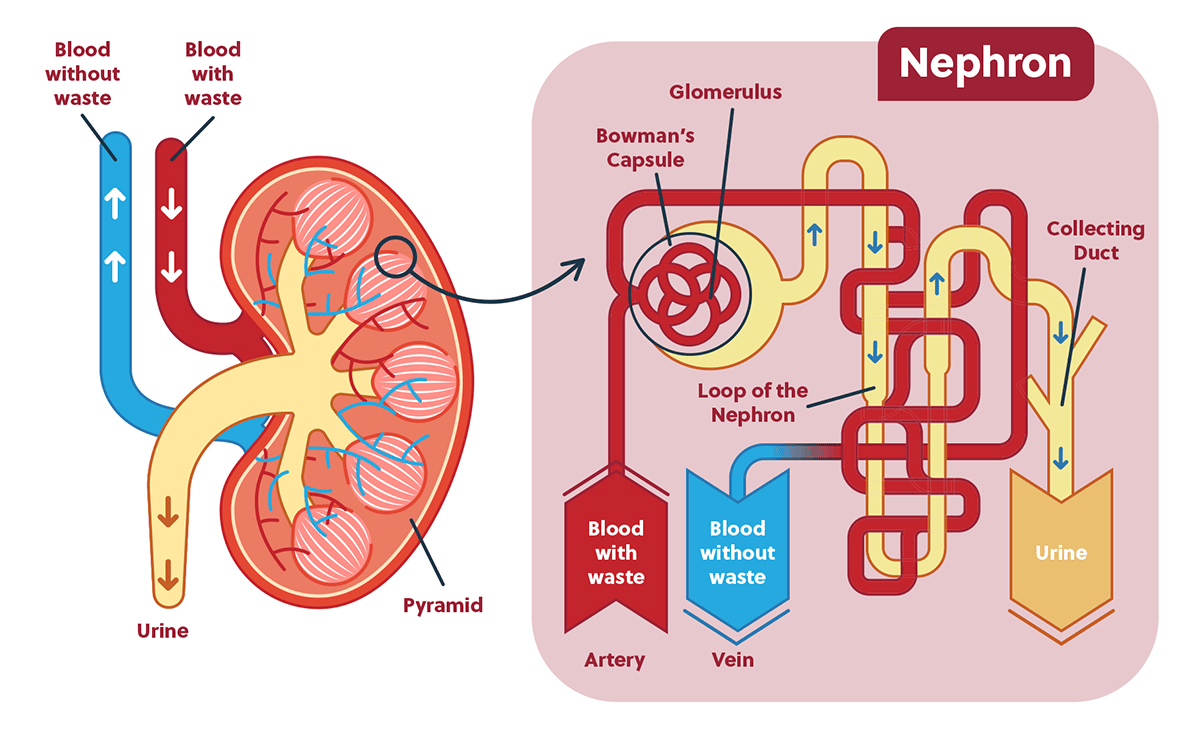
They never stop working. Despite the fact that people typically eat and drink three times a day, a process that can significantly affect the chemistry of blood and cells, the kidneys prevent the blood chemistry from changing by excreting electrolytes, water and organic substances through urine.
Unfortunately, in patients without kidney function, whatever they eat and drink remains in their bodies. In such patients, nephrologists need to control what the kidneys would normally do by artificially removing the necessary amount of water and electrolytes during dialysis treatments.
Briefcase-Sized Artificial Kidney
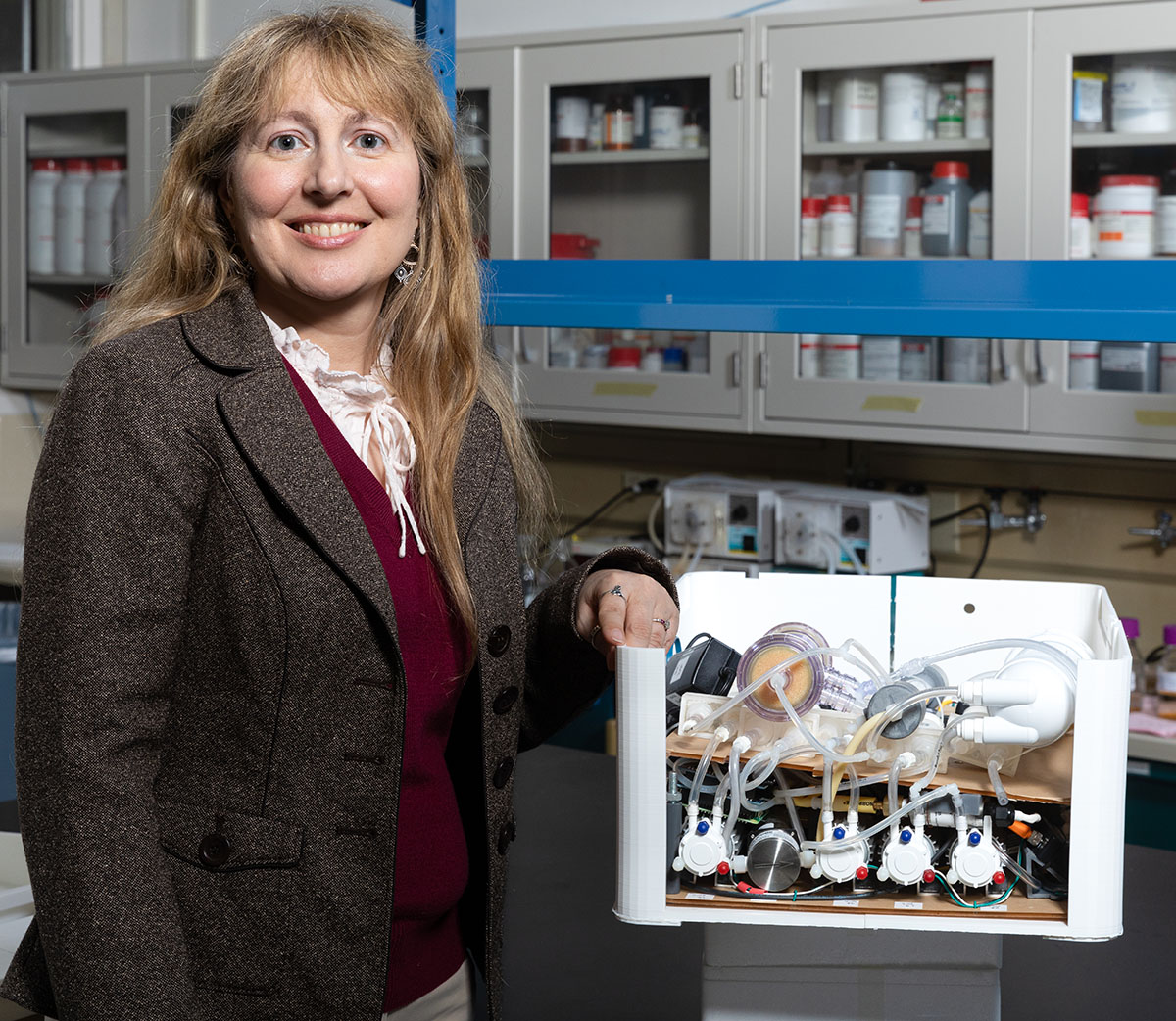
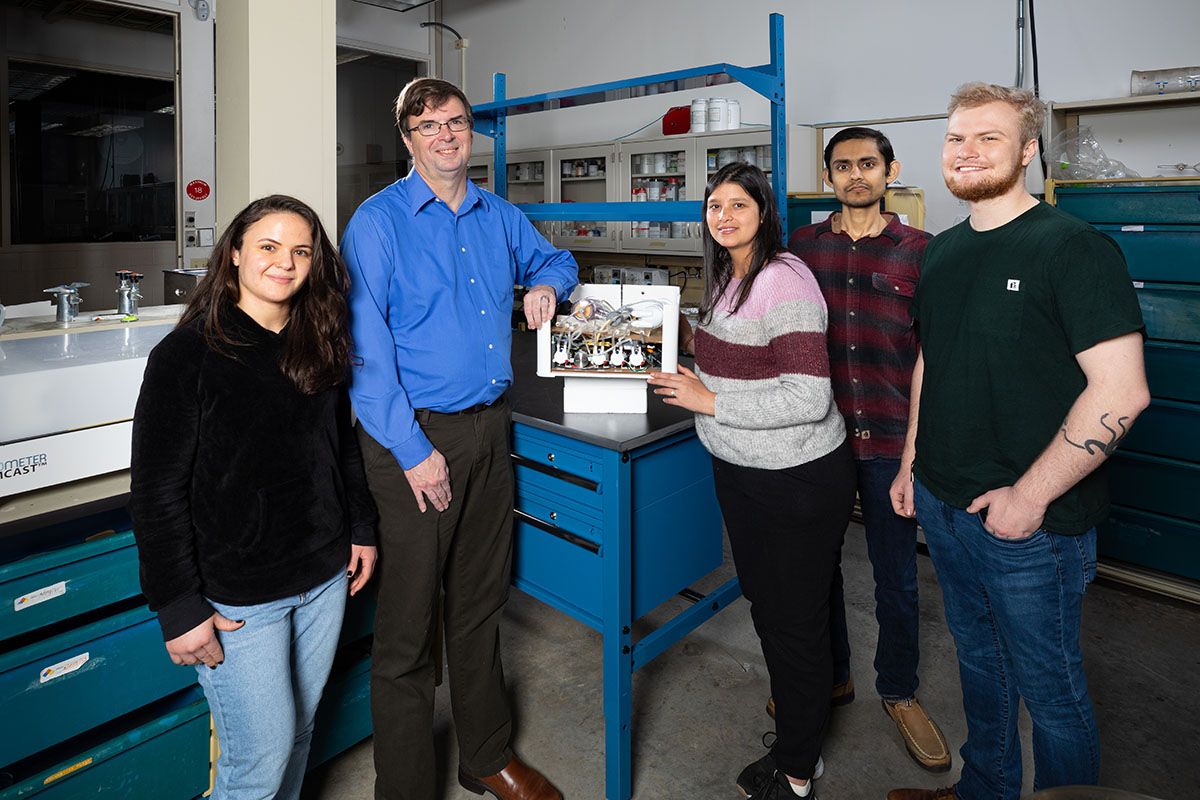
Creating an artificial device that performs the above functions is an immense and complex task, but the initial call from Kurtz led to a fruitful collaboration. In addition to Jamie Hestekin and Kurtz, the team also includes Christa Hestekin, associate professor of chemical engineering, and US Kidney Research Corporation, whose Founder/CEO is Roland Ludlow.
US Kidney Research Corporation, based in California, supports this research and plans to market the world’s first tabletop artificial kidney, based on a prototype that will ultimately be developed by the Kurtz-Hestekin-Ludlow team.
With $4 million in funding from the company, the research team, including students in the Hestekin laboratory, are building a prototype device that fits on a desktop. It could be used at work or placed on a bedside table and used while a patient sleeps.

“A key difference between our artificial kidney and dialysis is that dialysis is a very passive transport method,” says Christa Hestekin. “Our system uses active transport in order to help control levels of the toxins within the body using electrodeionization.”

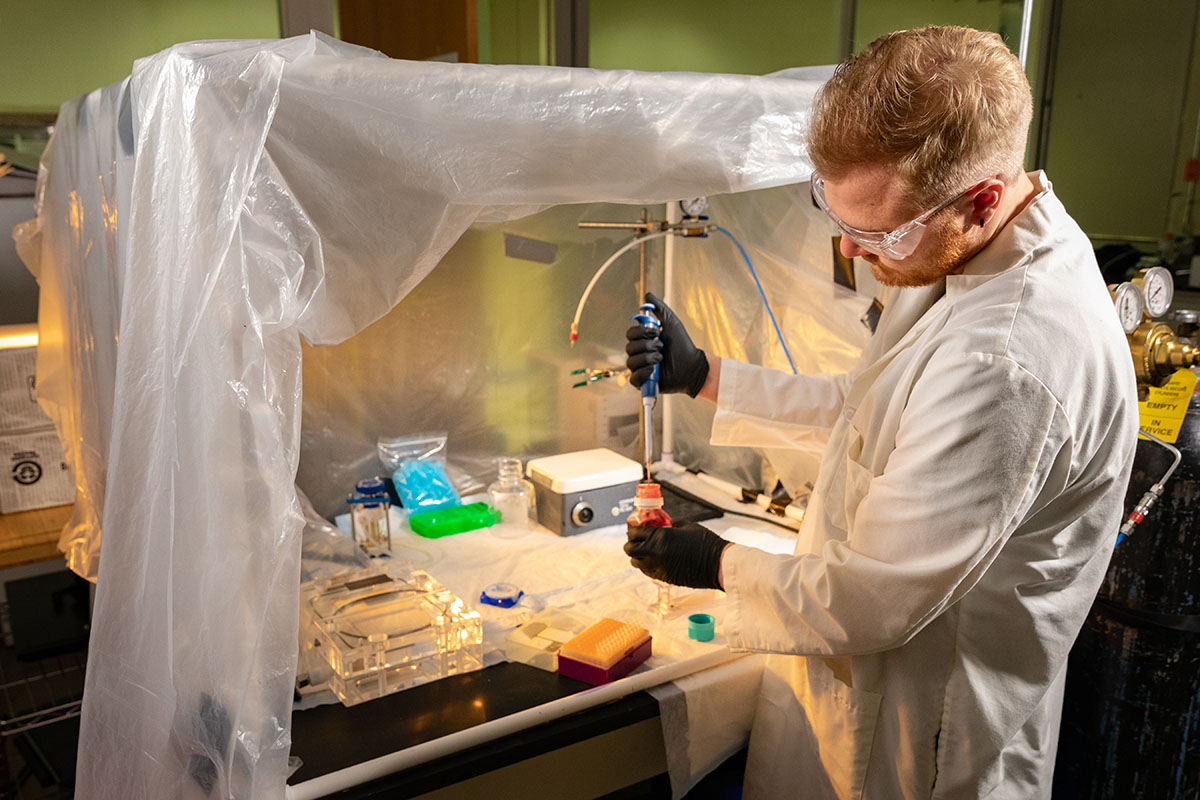
More recently, a secondary discovery has given the research team further reason to be excited. For a different project, Jamie Hestekin and students were experimenting with various types of membranes to use as friction material for surface engineering. They were having success with a membrane made of cellulose, and one student decided to try it on blood. This experimentation led to encouraging results and might address one of the challenges of using ultrafiltration membranes, which tend to clot. These membranes are currently used for hemodialysis, the primary treatment for people with end-stage kidney disease.
“This membrane looks more like nature,” Jamie Hestekin says. “It mimics the glomerulus and the tiny fibers connected to it better than anything out there.”
Working with students on these types of discoveries is a win-win for all parties involved.
“It’s our graduate students, our undergraduate students and our post-docs that are really in the lab doing the work that’s necessary for this, and the company has been very supportive of our students by having them present and talk about what they’re doing for their own professional development,” Christa Hestekin says. “Dr. Kurtz has had regular sessions to teach them about nephrology and how the kidney actually works.”
The researchers have used the cellulose membrane in animal studies, but it has not yet been tested as part of the artificial kidney device. There is potential to integrate it into hemodialysis dialyzers, because its filtering performance is superior to those currently in use. US Kidney Research Corporation has licensed the membrane for this purpose and is exploring potential collaborations.
Making Research Meaningful
Developing and marketing an artificial kidney could give patients with kidney disease more options and independence, while potentially reducing Medicare expenditures significantly. Patients using the device would no longer need to visit a dialysis clinic three times a week for treatment. And because their treatment would be done daily at home or in the office, with less stress on the cardiovascular system, there would likely be improvements in both patient quality of life and lifespan.
 Arkansas ranks 3rd in the nation in kidney disease deaths.
Arkansas ranks 3rd in the nation in kidney disease deaths.
“The money savings could be tremendous,” Jamie Hestekin says.
The environment could also potentially benefit. Billions of gallons of wastewater produced annually by dialysis treatments would no longer enter water treatment facilities, and development of a waterless artificial kidney would significantly reduce the carbon footprint associated with using and manufacturing water-purifications systems, dialysate solutions and dialyzers. The advantage of not using water means the system would be optimal in countries where water is scarce.
Ultimately, the team would love to scale down components to create a partially or fully implantable device, which would be about the size of two fists.
“We’re really putting something together that’s going to be useful for peoples’ lives,” Christa Hestekin says, and Jamie agrees: “In addition to the great scientific contributions from this, we are really helping to solve a problem.”